Physician,
anneal thyself
Stress appears to be an inescapable part of the practice of healthcare, but is a focus on building resilience the best solution?


David Alderson
Consultant ENT Surgeon, Torbay and South Devon NHS Foundation Trust
I ’m not really a sporty person, but I like walking, cycling and open-water swimming – keeping fit, keeping healthy, mostly just enjoying the countryside where I’m blessed to live. Some time ago I was given a sports watch: it measures my heart rate, tracks my routes and even tells me the time. I love it.
The watch indicates how hard I’ve been exercising (stress), but also how much I’m being stretched (strain) and compares this with a longer term indicator of my coping ability (tolerance). A simple display shows where I am on my journey.
I wish there was a watch to measure the stress, monitor the strain, display the tolerance of those working in healthcare: a wearable tech portrait of nurses’ and doctors’ mental health and wellbeing.
Stress appears to be endemic in healthcare. The causes are legion and a degree of stress is, perhaps, an inescapable part of what it means to be a doctor or a nurse. It’s difficult to say whether stress has risen or we are becoming more attuned to its toll at the human level, to the strain. Studies show high rates of burnout, of compassionate people unable to continue in their roles, of caring individuals unable to carry on.
Time to get tough
Many well-meaning initiatives have tried to build better resilience in healthcare staff to help them cope with the inevitable stresses they will experience. The term started to be applied in the 1970s, but the concept dates back much further. It underpinned, for example, the efforts of the combatant armies in the First World War to find ways to return psychologically damaged soldiers to the trenches. This idea of patching up wounded individuals and sending them back to face the guns amid worsening conditions, whatever the cost – and with no sign of progress towards an armistice – remains a common conception of resilience among those on the frontline of healthcare.
“It is counterproductive to ask physicians to ‘heal themselves’ through superhuman levels of resilience even as the practice environment continues to deteriorate1.”
Perhaps we can better understand the limitations and the antagonism by examining the underlying metaphor. Resilience is a term borrowed from materials science – a measure of how much stress (force) can be absorbed for a given level of strain (stretch).
A steel girder supporting a bridge will lengthen with increasing traffic. Within working limits the girder will stretch in proportion to the number of cars. When they leave the bridge it will spring back to its original dimensions and properties. A resilient girder will stretch less for the same weight of traffic.
However, increase the vehicles on the bridge beyond healthy limits and the girders will experience permanent, non-elastic deformation. Passively reducing stress is no longer enough: for the girder to regain its shape it needs an active process of remodelling. Continue to drive HGVs onto the carriageway and eventually the girder will fail.
“It is counterproductive to ask physicians to ‘heal themselves’ through superhuman resilience”
It might seem that the answer is to increase resilience so that the girder can cope with more stress. Quenching is the process of heating then rapidly cooling metals to increase their resilience. The resulting girder will certainly be very hard and there will be little in the way of external signs of strain as the stress load increases. But it will also be extremely brittle and will fail catastrophically, and without warning, as it reaches its limit.
For girders, better by far to increase toughness, which combines the elastic and non-elastic portions of the stress-strain curve, by annealing: careful heating beyond the recrystallisation point, then gradual cooling under controlled conditions. The overall ability of such girders to withstand stress – their toughness – far exceeds that of resilient, but brittle, quenched steel. And an annealed girder will deform as it approaches its yield point, demonstrating the need for both stress reduction and active processes to reconstitute its strength.
Resilience is futile
So where does that leave those working in healthcare and those wanting to help them? The stresses of healthcare can take us well beyond the point of elastic rebound. The situations we encounter and the experiences we share can change us permanently. Cyclical loading and chronic unrelieved stress will add to the damage, and the way we deal with these crisis points will strongly influence our ability to continue.
Traditionally, we have used quenching to battle-harden our frontline staff: “It happens”; “Man up”; “Feel free to cope.” And every day I see the brittle resilience that results: colleagues who can take anything the working day might throw at them until suddenly they can’t. Debriefing in all its forms has become our standard response to stressful events, yet it may actually promote burnout and dropout.
“Psychological debriefing should not be used for people exposed recently to a traumatic event,” according to a WHO recommendation in 2012.
On the other hand, the annealing properties of creative self-reflection are increasingly acknowledged: traumatic experiences, carefully revisited, can increase tolerance for the difficult times ahead.
“Creativity is a basic human response to trauma and a natural emergency defence system2.” Reflection can be much wider, and far deeper than the simplistic templates and cycles imposed by portfolios and appraisals: finding meaning through storytelling, making sense through creative writing, uncovering perspective through literature, allowing healing through informal discussions with peers and partners, or through counselling.
We can learn to recognise the signs of distress – in ourselves and our colleagues – as we approach the yield points of our professional lives; we can openly share these indicators and heed the need not only to reduce stress but find ways to remodel ourselves. For some, remodelling might come through engagement with life outside clinical practice: with faith, family, friends; exercise, gardening, cooking; art, writing, music. Others may need time away from stress. For some, professional help may be essential. I believe we are starting to see all these as normal, healthy, usual responses to the situations in which we work.
Resilience, toughness, tolerance: all these terms are problematic and none is a panacea for the effects of stress. But an emerging culture that turns away from quenching – and towards annealing – represents an important starting point.
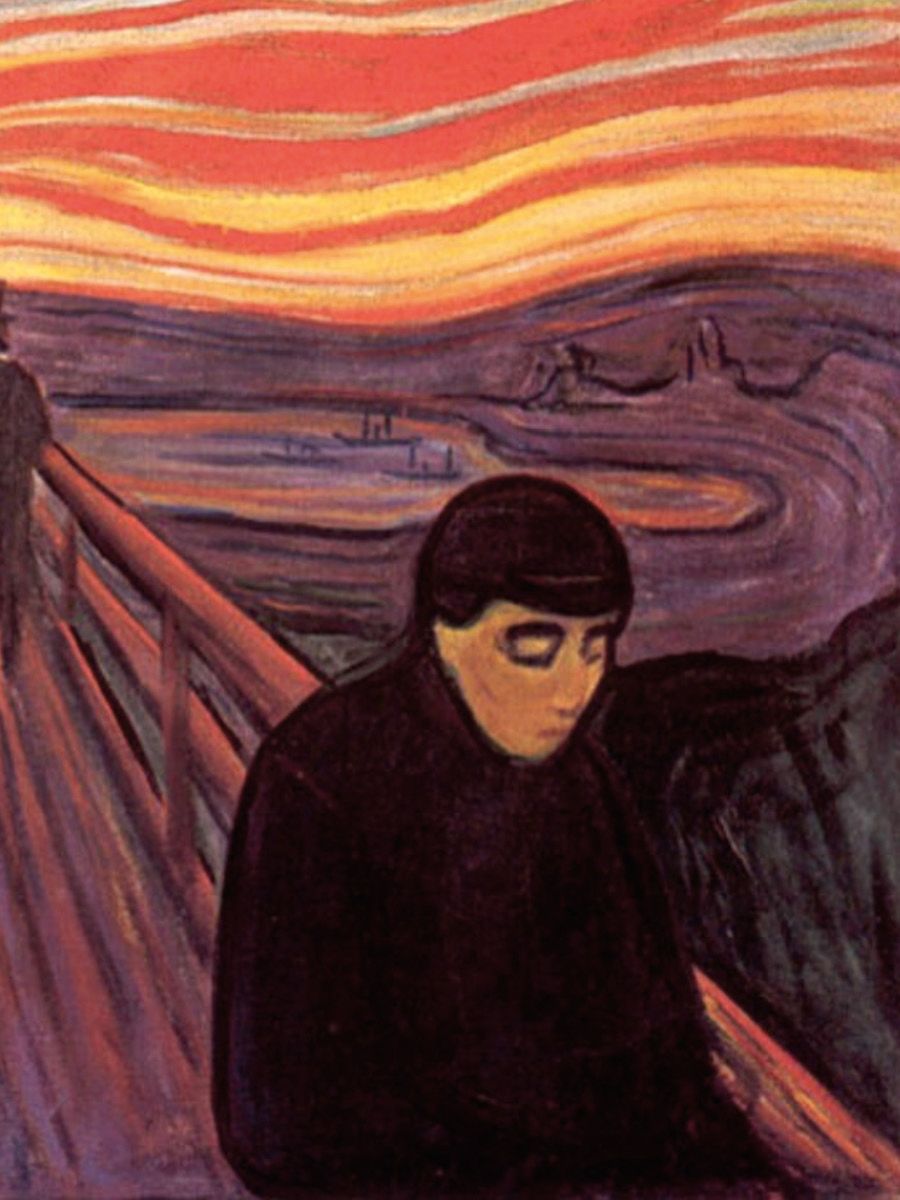
Picture of distress
Norwegian artist Edvard Munch created perhaps the best-known pictorial representations of inner distress. Walking with two companions by the side of a fjord in Oslo, he was overcome by his surroundings. He wrote: “My friends walked on. I stood there trembling with anxiety and I felt a great, infinite scream through nature.”
He spent years trying to portray the turmoil he had experienced: first, in Despair; later, in the various versions of The Scream. But this moment of breakdown didn’t spring from nowhere; his earlier paintings depict an ongoing, inner struggle – with childhood loss, with repeated rejection, with little in reserve to cope with life’s traumas.
|
References 1. Bohman B, Dyrbye L, Sinsky CA, et al. Physician well-being: the reciprocity of practice efficiency, culture of wellness and personal resilience. NEJM Catalyst 2017; 3(4). 2. DeSalvo L. Writing as a Way of Healing: How Telling our Stories Transforms our Lives. Beacon Press; 2000. |