Hands-on training
Stuart J Fergusson reviews his Rural Surgical Fellowship ahead of work in the Shetland Islands


Stuart J Fergusson: Consultant Surgeon, Gilbert Bain Hospital, Shetland
Around three-quarters of surgeons in training express the intention to complete a Clinical Fellowship. These aim to enhance the clinical and operative skills of senior trainees, typically involving intense exposure to a subspecialty area of practice and improving employability.
For many years NHS Education for Scotland has offered Rural Surgical Fellowships, a bespoke opportunity for general surgeons to undertake peri-CCT training for subsequent use in one of Scotland’s rural general hospitals.
These hospitals are in isolated small towns unable to support a full range of surgical specialists. Rural general surgeons typically offer elective general surgery across subspecialty areas (including colectomy), straightforward urology and minor orthopaedics.
They supervise the emergency assessment and treatment of every kind of surgical case, which can include the operative management of hip and ankle fractures, ureteric stenting, scrotal explorations and very occasional emergency craniotomy or thoracotomy for life-threatening bleeds.
The skill set required is much broader than that taught in a standard UK general surgery training programme, so the Fellowship offers four months to two years of experience tailored towards the surgeon’s intended rural practice.
A sample week from
my Rural Surgical Fellowship
Monday: Trauma theatre – cases: hip hemiarthoplasty, tendon repair in foot, patellar tendon repair
Tuesday: General surgery theatre – cases: umbilical hernia repair, inguinal hernia repairs × 2, rectal EUA, Karydakis flap for pilonidal sinus
Wednesday: Breast theatre – cases: image-guided wide local excision, sentinel node biopsy (SNB) + LICAP flap, mastectomy + SNB + implant reconstruction
Thursday: Morning – admin; afternoon – urology outpatient clinic
Friday: Obstetric theatre – cases: elective caesarean sections × 4
Aberdeen to Zambia
Following a CCT in colorectal and general surgery I was proleptically appointed to the role of Consultant Surgeon in the Shetland Islands (110 miles north of mainland Scotland). In preparation I undertook a Rural Surgical Fellowship from August 2021 to July 2023 at Aberdeen Royal Infirmary. The Fellowship incorporated monthly weekend locums on Shetland, where I was mentored by existing surgical colleagues, and a visit to a remote and rural hospital in Zambia.
My training time was focused on trauma/fracture management and core urology, including transurethral resection of prostate (TURP) and bladder tumours. I undertook regular work in general surgery to enhance and maintain existing operative and endoscopic skills. Additional time was spent in obstetrics, paediatric surgery, neurosurgery, ENT, ophthalmology and cardiothoracics.
This meant attendance at many outpatient clinics, multidisciplinary team meetings, operating lists and teaching sessions. After initial modular placements, I was able to target optimal learning opportunities on a day-by-day basis, resulting in a hugely varied working week, as illustrated in ‘A sample week from my Rural Surgical Fellowship’ (opposite page), which is an extract of a week from my year-two diary.
Bring on the case load
At the conclusion of my Rural Surgical Fellowship I had participated in 810 procedures (summary in Table 1) and undertaken 32 procedure-based assessments, documenting readiness for independent practice in hip hemiarthoplasty, cannulated hip screw, tendon repair, ankle fracture fixation, carpal tunnel decompression, TURP, transurethral resection of bladder tumour (TURBT), optical urethrotomy, circumcision, hydrocele and orchidopexy.
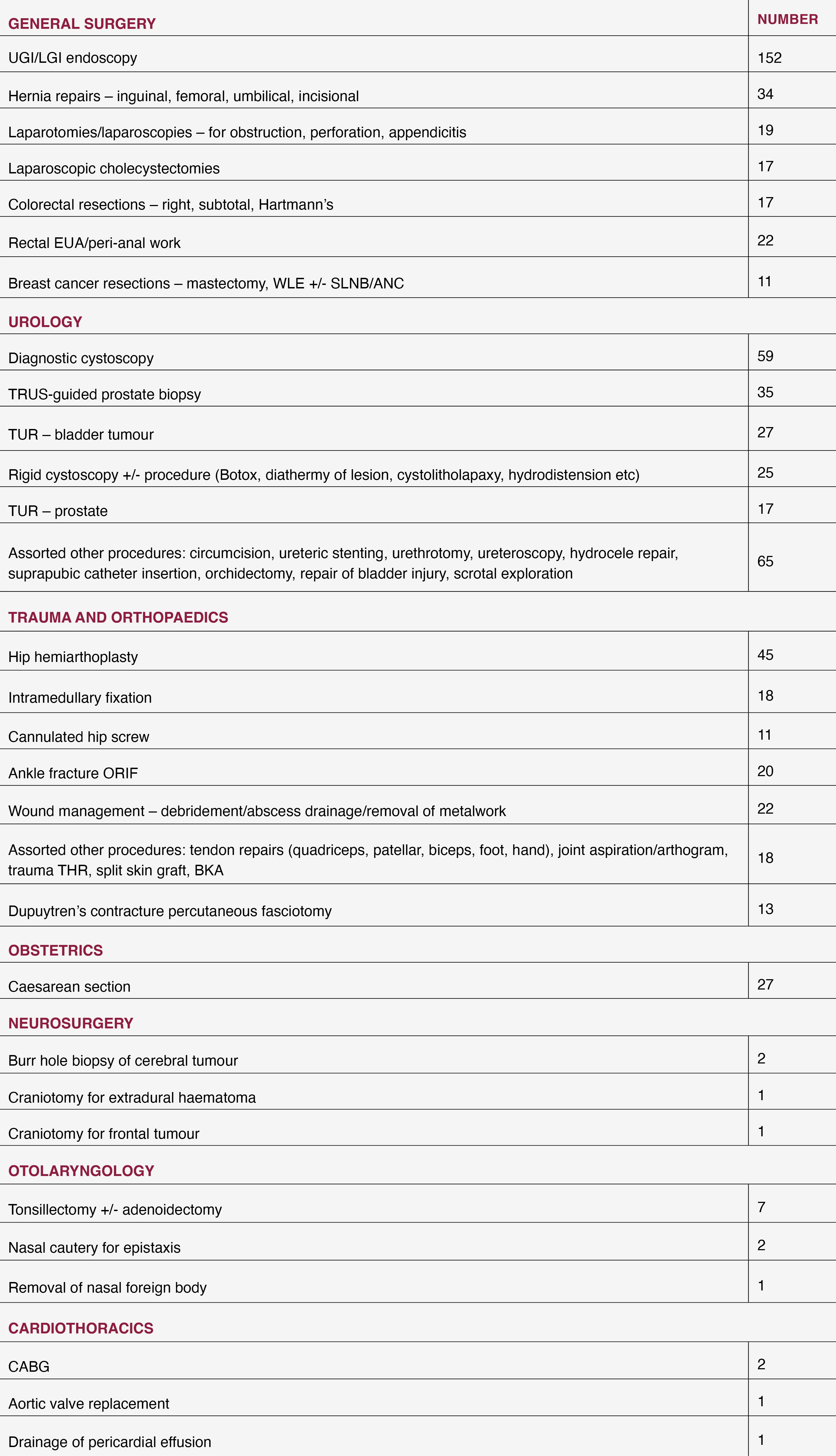
Table 1: Abbreviated logbook summary
Table 1: Abbreviated logbook summary
The time spent in this Fellowship was hugely enjoyable and productive. I am credentialed to be able to offer a high-quality service on Shetland as an extended-range surgical generalist, maintaining services on the island and avoiding expensive and time-consuming transfers.
The RCSEd’s Faculty of Remote, Rural and Humanitarian Healthcare aims to “improve the health outcomes of individuals living and working in remote, rural, austere and life-threatening areas of the world”, and the key challenge in this objective is the lack of healthcare workers in rural environments.
I believe my Fellowship experience demonstrates that even in this modern era of highly specialised training within tight boundaries, well-targeted broad training and a can-do attitude can create the generalists required for rural communities.
I am grateful for the Faculty’s support in raising awareness of this training opportunity.
This is a shortened version of an article available on the College website, rcsed.ac.uk.
|
References Find a full list of references click here. |