Platelet concentrates are classified based on preparation methods
Platelet concentrates are classified based on preparation methods
Platelet-rich plasma and platelet-rich fibrin in oral surgery: a narrative review
This article focuses on the effectiveness of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in various oral surgery procedures. Both PRP and PRF are derived from the plasma fraction of autologous blood and contain a high concentration of platelets, which are rich in cytokines and growth factors that aid the healing process.
PRP and PRF have several potential applications in oral surgery due to their regenerative properties. They are primarily employed to accelerate healing in dental extractions, implant surgeries and for patients undergoing bisphosphonate-related treatments. These products support tissue regeneration, reduce inflammation and promote healing.
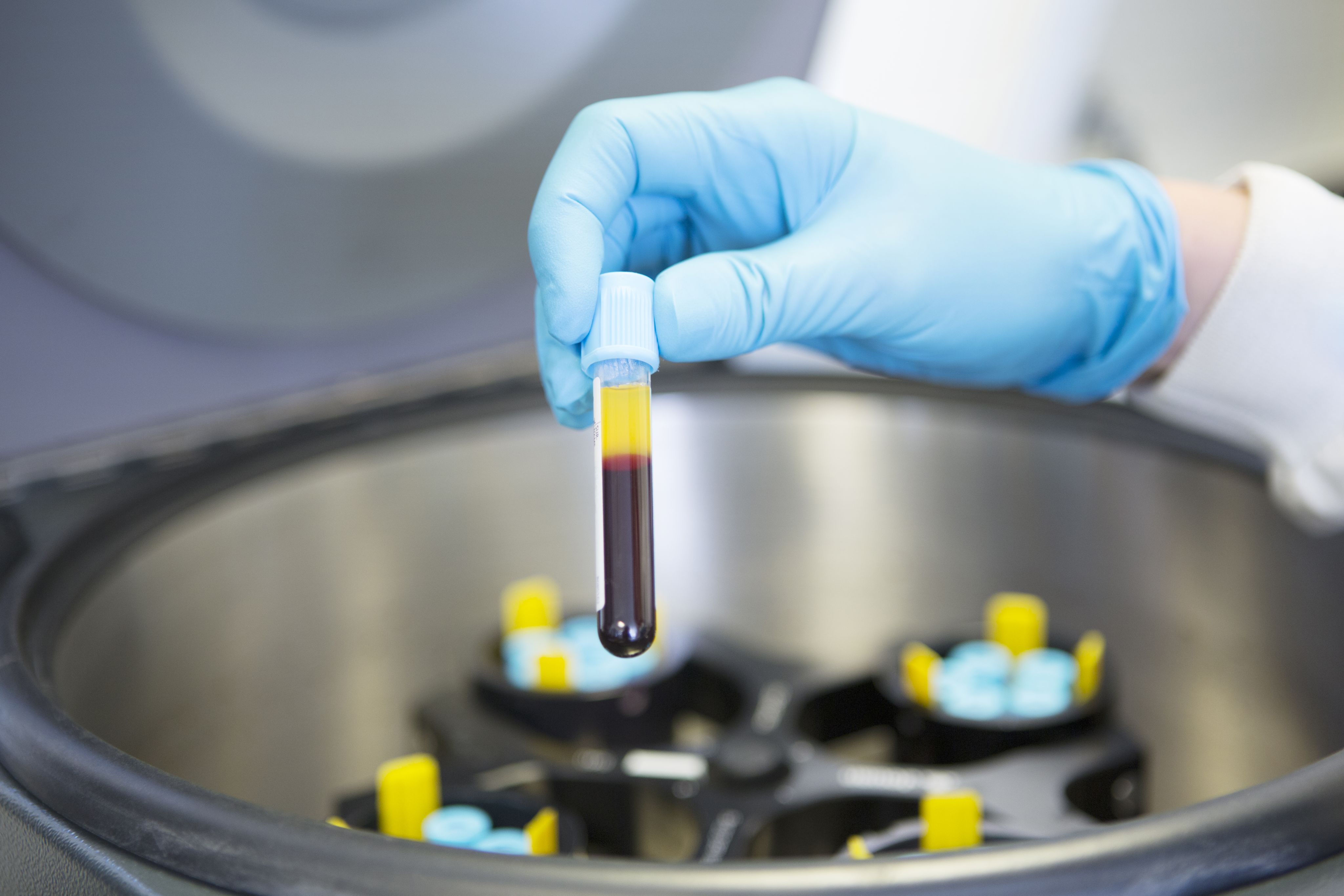
Platelet concentrates are classified based on preparation methods and biological composition. PRP and PRF can be either pure or leukocyte-rich. Each type of concentrate has distinct properties that influence its usage in dental procedures. PRF, in particular, is commonly used in various oral surgeries due to its fibrin-rich architecture, which enhances tissue regeneration and healing.
Several studies examined in the review, when considering the removal of third molars, show that the application of PRF significantly reduces postoperative pain, accelerates soft tissue healing and can result in reduced swelling. However, the authors conclude that there is a lack of randomised controlled trials to support the use of PRF after the removal of third molars.
The review discusses studies that highlight PRF’s effectiveness in reducing the incidence of alveolar osteitis – noting one study which found that patients who received PRF after extractions had significantly lower pain levels and faster epithelialisation compared with the control group. Similarly, other studies confirm that PRF application decreases the occurrence of dry socket.
PRF has proven beneficial in implant surgery, particularly for immediate implant placements, where it enhances the stability and osseointegration of the implants. PRF also aids in peri-implantitis treatment by promoting soft-tissue healing and bone regeneration, though more research is needed to solidify its effectiveness in this area.
PRF is also used in sinus-lift procedures, which are performed to increase bone volume for implant placement in the maxillary region. However, the benefits in terms of reduced postoperative complications like pain and swelling are not always statistically significant.
The review highlights the potential of PRF and PRP in managing medication-related osteonecrosis of the jaw (MRONJ). Several studies report successful outcomes in patients treated with PRF, including improved tissue healing and reduced pain. PRF promotes the formation of gingival tissue and accelerates healing after sequestrectomy (removal of necrotic bone), making it a promising treatment for MRONJ, though more large-scale studies are required.
The authors conclude the use of PRP and PRF in oral surgery presents promising results, especially in accelerating healing and reducing postoperative complications. However, there is a lack of standardised protocols for their use, and more high-quality, randomised controlled trials are needed to provide evidence-based guidelines. Despite these limitations, PRF and PRP continue to gain popularity due to their simplicity of use and regenerative benefits in various dental procedures.
Egierska D, Perszke M, Mazur M, Duś-Ilnicka I. Platelet-rich plasma and platelet-rich fibrin in oral surgery: a narrative review. Dent Med Probl. 2023;60(1): 177–186.
Platelet-rich plasma and platelet-rich fibrin have regenerative properties
Platelet-rich plasma and platelet-rich fibrin have regenerative properties
The effectiveness of autologous plateletconcentrates in prevention and treatment of medication-related osteonecrosis of the jaws (MRONJ): a systematic review
There is currently no standardised, definitive treatment protocol within the literature where established MRONJ is concerned. The role of autologous platelet concentrates (APCs) in management of MRONJ has been investigated due to their soft-tissue regenerative properties through the release of growth factors, which may encourage mucosal healing.
This systematic review explores whether the adjunctive application of APCs is effective in preventing and treating MRONJ. A literature search was conducted across four databases. Thirty articles were ultimately included evaluating both prevention and treatment strategies – eight articles focused on the prevention of MRONJ with APCs and 23 focused on MRONJ treatment. One article was included in both groups. The risk of bias was assessed in line with the recommendations of the Cochrane Collaboration and GRADE working group. Meta-analysis was performed for systematic reviews.
A 92–100% success rate was reported in the studies included when APCs were used as a preventative strategy. The most commonly prescribed drugs in this group were zolendronate IV (51%), alendronate PO (19%) and denusomab SC (11%). Success was defined in all studies as complete mucosal coverage with no visible exposed bone. Penicillin-based antibiotic therapy was recommended both pre- and post-treatment by all studies. Overall, the authors report that the adjunctive use of APCs may be an effective method of preventing the development of MRONJ in approximately 86.13% of cases (p < 0.001)
However, less clarity was offered on the use of APCs in treatment of established MRONJ. The authors found no statistical significance for treatment (83.4%, p = 0.08) with the application of APCs. Again, zolendronate IV, alendronate PO and denusomab SC were the most prescribed drugs in descending order respectively.
There was no consistent definition of success in the studies included – varying between lack of bone exposure, complete mucosal healing, lack of pain or no recurrence – and there
was a high level of heterogeneity between the studies both in design and surgical protocols described.
With regard to the type of APC used, the studies selected do not definitively promote the use of one APC in comparison to another. However, the authors do note that PRF formulations had multiple superior characteristics in comparison to PRP, including cost-effectiveness, ease of production and use, wound-healing potential and no addition of anticoagulant being required. Therefore, they concluded that PRF may be the preferred APC formulation for MRONJ management.
Overall, this review emphasises the need for high-quality randomised controlled trials to further evaluate the use of APCs in the management of MRONJ, but does highlight the promise that APCs show, especially in the possible prevention of MRONJ.
Nowak SM, Sacco R, Mitchell FL, Patel V, Gurzawska-Comis K. The effectiveness of autologous platelet concentrates in prevention and treatment of medication-related osteonecrosis of the jaws: a systematic review. J Craniomaxillofac Surg. 2024; 52(6): 671–691.
Read more