Manchester: respecting the recommendations
Two years on from being cited to provide a statement to the Manchester Arena Inquiry, the Faculty of Pre-Hospital Care remains committed to driving forward its monitored recommendations
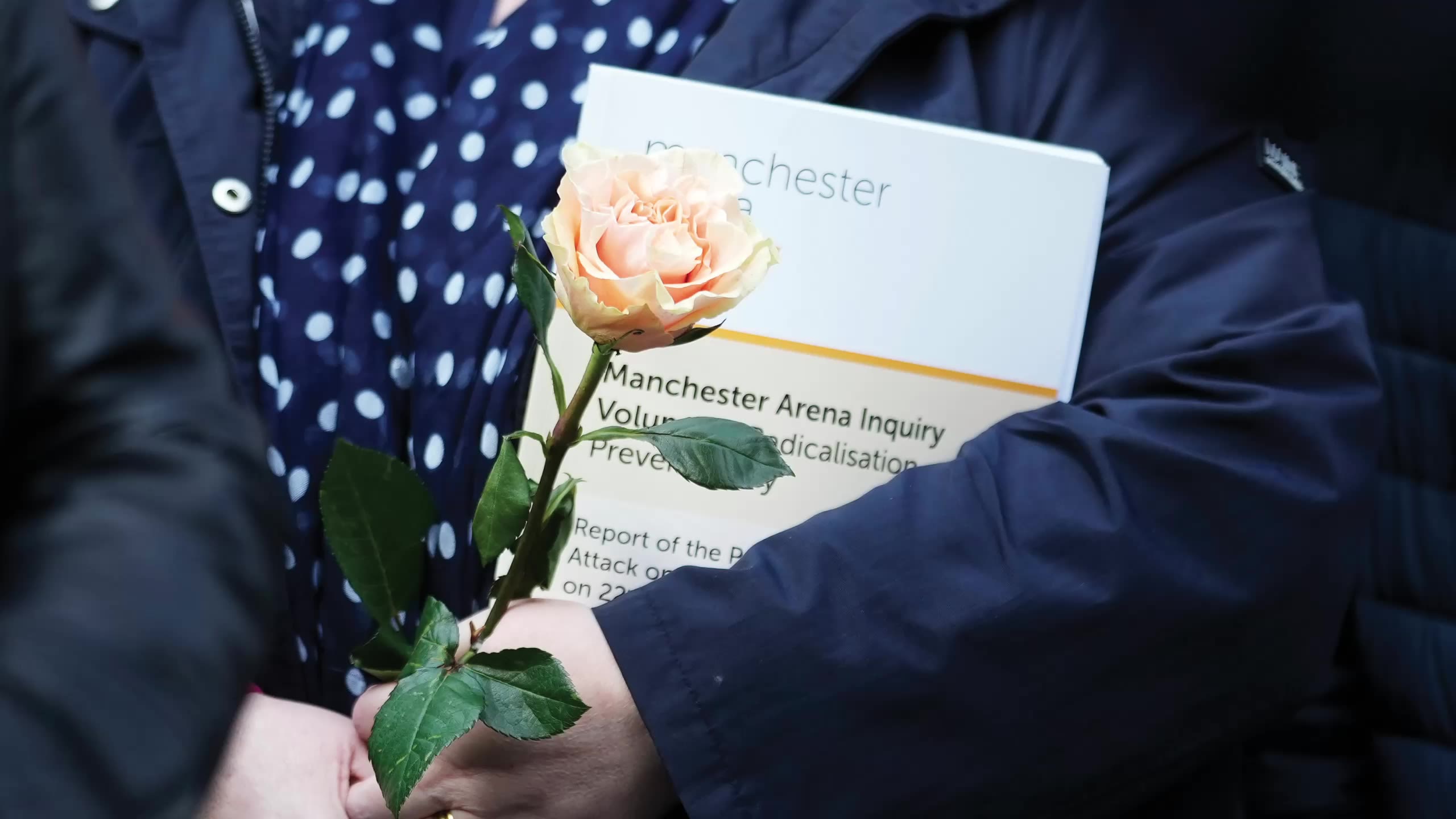
On 22 May 2017 a suicide bomber detonated an improvised explosive device in the Manchester Arena, killing 22 and injuring over 900 people.
During the subsequent public inquiry, chaired by the Hon Sir John Saunders, the response by the emergency services was closely examined. In Volume Two of the inquiry report, Sir John concluded that, “looked at overall, and objectively, the performance of the emergency services was far below the standard it should have been”1. The report went on to make 149 recommendations relating to the emergency services – many of the things that went wrong during the response to the Manchester Arena incident had gone wrong before.
Dr Kevin Pollock’s report, Review of Persistent Lessons Identified Relating to Interoperability from Emergencies and Major Incidents since 1986, carried out four years before the Manchester bombing, had previously stated: “… lessons identified from events are not being learned to the extent that there is sufficient change in both policy and practice to prevent their repetition”2.
Issues with interoperability between emergency services was one of those persistent themes. The Pollock report was one of the main drivers that led to the Joint Emergency Services Interoperability Programme (JESIP). Manchester Arena was the first major scrutiny of JESIP following a major incident involving a high number of deaths. A panel of joint emergency service experts, instructed by the Inquiry, reviewed the application of JESIP by the emergency services during their response to the arena attack and concluded: “JESIP substantially failed in all organisations.”3
In 2023, the Chair of the Faculty of Pre-Hospital Care (FPHC) was cited to provide a statement to the inquiry in collaboration with the College of Paramedics (CoP), the National Ambulance Resilience Unit (NARU) and the Department of Health and Social Care (DHSC).
The FPHC was required to comply with the legally enforceable requests of the statutory inquiry and found itself intricately involved and on extremely tight deadlines.
Collaboration is a core function of the FPHC and this dovetailed with a central tenet of the recommendations of the Inquiry. Some of our members had been involved in the delivery of clinical care on the ground on the night of the bombing, others had already contributed significantly to the Inquiry and some had subsequently been invited to collaborate on projects resulting from Volume 2-1 of the Manchester Arena report.
The questions posed to us from the Inquiry required thorough scrutiny of the history of the Faculty, its aims, roles and constitution, describing a remit that has vastly evolved over recent years. As well as being central to the GMC-recognised sub-specialty of Pre-Hospital Emergency Medicine (PHEM), the FPHC was well placed as a multi-level and multi-professional Faculty, representing responders ranging from those delivering vital basic first aid, often the most crucial intervention, right through to those providing enhanced critical care. It highlighted to us the extensive number of agencies and organisations with whom we already worked closely, the multiple workstreams we support, and standards we set through our consensus statements and assess by our examinations.
FPHC mission, aims and objectives
- To set and maintain standards in pre-hospital care.
- Effectively integrate the efforts of all participants in pre-hospital care.
- Engage in development of clinical policy.
Our detailed statement to the Manchester Arena Inquiry (MAI) can be found by scanning the QR code.
But what next? It does not, and must not, end there. What did we learn and how can we do better?
Sir John Saunders stated: “Many of the responders from the Emergency Services who bravely rushed to the scene of the Manchester Arena bomb did not know what they could do to best assist the victims. The evidence at the Inquiry showed how vital it is that the best possible treatment is available during the ‘care gap’, that is the time between when life-threatening injuries are suffered and the victims arrive at hospital for treatment, in order to save lives and reduce the long-term effects on those who survive.”
The concept of the ‘care gap’ had been a persistent theme in previous Inquiries. It is the term given to the delay in clinical care being provided to casualties who have been injured in a high-risk major or complex incident and was a key focus of the MAI.
The recurrent failure to adequately learn lessons, with a consequent impact on patients, reached a pivotal point following the MAI. The Faculty, in association with a range of other bodies, is now in the middle of a fundamental re-examination of how the emergency services respond to major and complex incidents within the United Kingdom. We committed to take many of the monitored recommendations forward, with Faculty members invited on to several task and finish groups and the Chair being co-opted on to the NHS England Strategic Oversight Group.
The NHS has established the Clinical Response to Major Incidents Programme (CRMI), the aim of which is to produce an auditable, national service specification for the delivery of patient-focused clinical care at major incidents. There are already some significant outputs making a positive impact on day-to-day patient care and bringing the added benefit of familiarity to frontline staff in the event of a major incident:
New NHS triage systems – Ten Second Triage (TST) and the Major Incident Triage Tool (MITT) – which have been adopted widely across pre-hospital clinical practice and other emergency service responders.
A successful clinical trial of pre-hospital lyophilised plasma utilisation by NHS paramedics is improving the administration of blood products in complex emergencies.
Administration of tranexamic acid via the intramuscular route has led to its introduction into Joint Royal Colleges Ambulance Liaison Committee guidance and progress is being made on a smaller volume injection and an autoinjector option.
More widely available and rapidly administered analgesia options.
However, the CRMI programme is taking things much further and will include a fundamental review of pre-hospital command, including evaluations of a new ‘clinically focused command model’. It is exploring the feasibility of a ‘default to deploy’ model for frontline clinicians to reduce the care gap and is working collaboratively with multi-agency partners to develop ‘command discretion’ allowing a risk-based assessment of when to deviate from protocols. Pre-hospital clinical practitioners will make a positive contribution to this discussion because they are accustomed to working within clinical practice guidelines but also using their professional judgment to adapt interventions or treatments
to meet the individual needs of patients within a wide range of pre-hospital challenging circumstances.
The FPHC is a key stakeholder within the NHS CRMI programme. It is directly supporting several of its workstreams aimed at producing optimal clinical guidelines and pre-hospital care pathways for the mechanisms of injury arising from the types of incidents detailed in the UK National Risk Register4 for major and complex incidents.
The Diploma in Major Incident Management is open to doctors, nurses, paramedics and others
The Diploma in Major Incident Management is open to doctors, nurses, paramedics and others
The MAI statement also gave us another opportunity
The Diploma in Major Incident Management (DipMIM) had been in development for many years and became a key element of the MAI statement, articulating the concept of a multi-professional standard for the provision of an emergency response. The concept was inspired by the vision of FPHC members and previous tragic events both in the UK and internationally, with the ultimate catalyst being the MAI. In close collaboration with RCSEd, the work to comply with the Inquiry helped us finally launch the DipMIM, supported by Sir John Saunders.
The exam is the end product of a vast amount of work and time provided voluntarily by a small group of members, many of whom are national experts in major incident management and who have daily involvement in improving future responses to major incidents. The DipMIM is a key component in addressing the care gap and the need for close collaboration between agencies and responders at the scene of any future incident to maximise care.
Crucially, the exam is open not only to doctors, nurses and paramedics but also to all those who may be involved in the planning for, or organisation of, a major incident response above that of their own area of professional expertise. The emphasis is on the organisational and regulatory framework of major incident management, is consistent with the Faculty’s aims of setting standards, and reinforces the FPHC’s position as a leading player in the field, both nationally and internationally. The credential is increasingly important in the current context of heightened terrorist threats and the evolving nature of Emergency Preparedness, Resilience and Response (EPRR). Success in the DipMIM will confirm a candidate’s competency and experience at a level consistent with effective leadership in emergency response and readiness.
Dr Paul Hunt, Deputy Convenor for the Diploma, says: “The DipMIM encourages joint working across professions and specialties by establishing a core and recognised level of knowledge. We hope that, in time, this Diploma will become a prerequisite for those undertaking such duties.”
The Diploma represents a significant step forward in professionalising the response to major incidents. It offers a much-needed qualification that will elevate standards for emergency response management and build resilience. As the world faces an evolving landscape of challenges, the DipMIM sets a new standard for preparedness and leadership in major incident management. We owe it not only to the victims and their families, but also to all responders, to ensure that responders have appropriate knowledge, standards and training.
The DipMIM was always intended to be a key element in a broader strategy of cultural evolution, aiming to professionalise incident response. It also supports a ‘whole-life learning’ approach that includes all agencies and promotes the ethos of saving lives, preventing harm and working collaboratively.
The design and syllabus domains of the DipMIM were carefully considered and are aimed at improving coherency and collaboration across all disciplines and responder/provider organisations. It fills an important space between the Major Incident Medical Management and Support (MIMMS) course and an academic degree in Major Incident Management. We are at a pivotal moment in the development of emergency service management in the UK and successful completion of the exam will, hopefully, occupy an increasingly prominent position in the development of decision-makers and commanders involved in managing complex or major incidents. It creates an examination underpinned by academic and professional rigour.
Sir John Saunders said: “As Chairman of the Inquiry, I am delighted that this Diploma is being set up. It will help meet one of my most important recommendations and assist in trying to ensure that the shortcomings in the emergency response at Manchester will not recur.”
The Faculty was invited to speak about its work at the launch of the NHS CRMI in Manchester in the presence of Sir John.
Dr Pam Hardy, Chair of the FPHC, said: “I was humbled by the feedback received and hope the launch of the Diploma serves to illustrate our commitment to the recommendations of the Inquiry, our willingness to learn, and our dedication to all those ever involved in such tragic circumstances.”
In addition to the work taking forward the recommendations of the MAI outlined above, we are heavily involved in other relevant initiatives and work strands relevant to major incidents.
Pre-Hospital Research and Audit Network (PRANA)
The Faculty is a stakeholder in the PRANA programme. We provide multi-professional support for collection, linkage and sharing of data, with the aim of developing an evidence base and national standard approach to many aspects of clinical care encompassing that delivered in a major incident setting.
Pre-Hospital Emergency Medicine (PHEM) workforce
The MAI explicitly recommended increased investment in consultant-delivered care to close the care gap in major incidents. This mirrored the recommendations by Lady Justice Hallett following the 7/7 London Bombings, which called for the enhanced deployment of doctors to incident scenes.
Unfortunately, the PHEM consultant workforce, and requisite training places, had been forgotten in medical training and overlooked in the recently commissioned Medical Training Review. However, our Intercollegiate Board for Training in Pre-Hospital Emergency Medicine has produced an 80-page workforce strategy document, focused on the long-term integration of PHEM doctors into consultant-level roles. This was created in response to a direct request from the Medical Director for Workforce Alignment in the Workforce, Training and Education Directorate of NHS England.
The document aims to influence long-term NHS workforce planning and address a growing national patient need for care from PHEM-trained consultants, a lack of funded training positions for PHEM consultants and a workforce gap.
Moreover, the role of PHEM consultants is expanding beyond scene-based trauma care, with services increasingly expected to deliver support for CRMI and EPRR frameworks by providing medical advisors, casualty clearing station medical leads or forward medical teams.
Event Healthcare
The Event Healthcare Standard, with a focus on establishing a standard for the level of healthcare services required at events, is being developed by the DHSC and NHS England following recommendations from the MAI Volume 2. Although the standard will be published as non-statutory guidance, there is potential for aspects of it to be considered for statutory guidance. Event healthcare was already one of the FPHC’s key strategic aims and we received an invitation from the DHSC and NHS England to contribute our “real-world expertise and experience so that the standard is effective and realistic”.
International support
In addition to delivering pre-hospital trauma care courses, the FPHC has been involved in disaster management training in India and Nepal for many years, working with the charity Saving Lives International and recently cooperating with the Worshipful Society of Apothecaries. More recently, we have been approached for support following the Air India Flight 171 crash.
FPHC psychosocial report: Valuing Staff, Valuing Patients
The FPHC commissioned this report, which is of great relevance to the support of all those involved in major incidents as well as the day-to-day care of our patients. We are now developing a Charter to support the recommendations of the report.
Looking after our staff and our patients in challenging and potentially dangerous pre-hospital environments is our passion and purpose.
Our conference on 10 and 11 November will showcase much of this work and the wider contributions of the FPHC to patient care (scan the code for details).
Scan for FPHC conference information
References
1. Saunders J. Manchester Arena Inquiry Volume 2: Emergency Response (No.2). London: Home Office; 2022. p. iv.
2. Pollock K. Review of Persistent Lessons Identified Relating to Interoperability from Emergencies and Major Incidents since 1986. Emergency Planning College Occasional Papers, Number 6. London: Civil Contingencies Secretariat, Cabinet Office; 2013. p. 19.
3. United Kingdom Home Office. Manchester Arena Inquiry: Emergency Service Experts Joint Capping Report. INQ035372. London: Home Office; 2020.
4. United Kingdom Cabinet Office. National Risk Register. London: Cabinet Office; 2025.
Read more