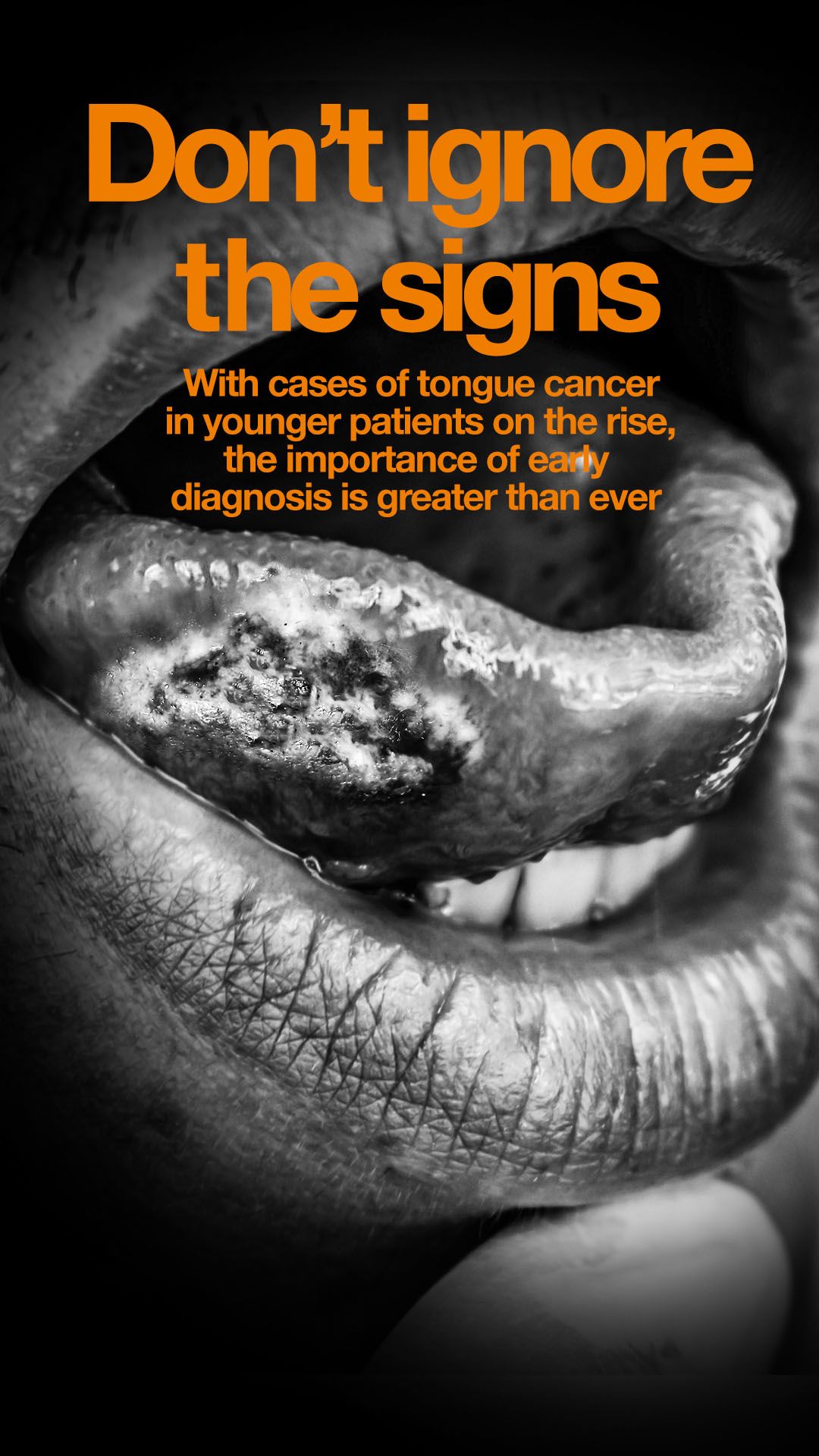
In recent years, there has been a concerning rise in the incidence of tongue cancer among younger populations. The results, published in Oral Oncology, show a significant increase in cases of tongue cancer in people under 45, particularly in women, where the incidence has risen by a staggering 385% over 32 years.
This alarming trend highlights significant patient safety concerns, especially related to the delayed diagnosis of tongue cancer in patients who do not present traditional risk factors, such as being older and male and having a history of smoking and high alcohol consumption.
Young Tongues is a charity at the forefront of addressing this issue – it is dedicated to providing support services to young patients with tongue cancer worldwide. Founded by young survivors of tongue cancer, it offers a platform for patients to share experiences, raise awareness and advocate for better diagnostic practices. Through the peer-to-peer support network, members have identified common issues and patterns that contribute to the delayed diagnosis of tongue cancer in younger patients.
A call to action
A primary concern raised by the community is the lack of awareness among both dentists and GPs of the rising incidence of tongue cancer in younger demographics. Many young adults report that their symptoms were initially dismissed or misdiagnosed by healthcare providers who did not consider tongue cancer a likely diagnosis because of the patient’s age and lack of traditional risk factors. Symptoms such as persistent sores, pain and changes in the tongue’s appearance were often attributed to less serious conditions, leading to dangerous delays in appropriate diagnoses and surveillance.
Chloe Gower-Page recalls her experience: “I was told there was no way my white patch, diagnosed twice as frictional keratosis, could turn into cancer. When the pain continued for more than five years and I was given a non-urgent referral that took six months, the biopsy showed squamous cell carcinoma (SCC).”
Michelle VanOpdorp experienced a similar delay. She had oral lichen planus inside her cheeks and complained for months to her dentists about a painful white spot on her tongue. She was eventually referred to an oral surgeon who refused to biopsy the spot, instead treating the oral lichen planus with steroids. Two months later, with more pain and the white spot now an ulcer, she demanded a second opinion. By the time the biopsy confirmed SCC, a second white spot had appeared on the other side of her tongue. “I was diagnosed with SCC cancer twice within a month,” says Michelle.
Barriers to diagnosis
Several factors contribute to the delayed diagnosis of tongue cancer in young people. A significant barrier is the misperception among healthcare providers that tongue cancer is unlikely in younger, non-smoking, non-drinking patients. This outdated view can lead to a lack of urgency in investigating symptoms. Also, the ongoing dental crisis exacerbates the problem because many patients struggle to access NHS dental care, resulting in prolonged symptoms and mismanagement.
Louise Hutchings shares her story: “In August 2020, I felt as though I had burned the side of my tongue. By September, I noticed a strange white and red patch in the same place. I didn’t think anything of it. By December, my sister convinced me to see someone. The GP suggested I get a dentist’s opinion, promising an urgent referral if needed. The dentist was not concerned, thinking it might be geographic tongue or lichen planus. Despite my worries, he reassured me it wasn’t cancer, saying: ‘Tongue cancer is an old drinking and smoking man’s cancer.’
“I decided not to pursue the urgent referral and instead waited for the non-urgent referral to go through. Because of Covid-19, my referral was delayed. In October 2021 the patch grew, and by February 2022 I started biting my tongue in my sleep, causing pain. By March, the patch turned into an ulcer, prompting me to seek a second opinion at a private hospital. The surgeon suspected erosive lichen planus but was concerned about the red and white tissue mix. He referred me back to the NHS for a biopsy. After a further delay, the biopsy revealed I had SCC.”
Missing the signs
The implications of late diagnosis in tongue cancer are severe. Advanced-stage diagnoses are associated with higher mortality rates and more aggressive treatment regimens. Treatments for advanced tongue cancer often involve invasive surgeries, radiation, chemotherapy and sometimes immunotherapy, leading to long-term health challenges, including losing the ability to eat, swallow and speak. These side effects can be debilitating, impacting patients’ social, professional and personal lives.
In a recent community discussion, the Young Tongues shared which side effects following treatment for SCC of the tongue impacted their daily life the most. Kelly McSorley reported how she hadn’t been able to eat solid food since completing treatment and relied on a G-tube for nutrition, while Matthew Naquin told of his struggles with chronic dry mouth, affecting his speech and ability to eat, so he avoids doing either in public. Louise Riley said she hadn’t taken a photo of herself in the past two years without hiding part of her face, as the changes to her appearance decimated her confidence. Maria Scott reported how radiation fibrosis caused her to lose the ability to support her own head. Jen Bowskill shared how she won’t be able to walk her youngest son to his first day of school after being told she had run out of treatment options.
Currently, early diagnosis is the only tool our community has to save lives and quality of life. Barbara Fountain, founder of Young Tongues, explains: “I knew I was rare to be diagnosed with tongue cancer at 32, but I didn’t realise I was also rare among my community. I was extremely lucky that my dentist followed best practice, resulting in a stage I diagnosis.
“Although the diagnosis and treatment were life changing, I can speak, eat and only have minor long-term side effects. It was only when the Young Tongues community grew that I realised how incredibly lucky I was and how most of my peers had to fight to be taken seriously by their healthcare practitioners. It’s important that the diverse voices of our community and our stories are heard to demonstrate the importance of early diagnosis.”
Better education
To address these challenges, Young Tongues advocates for comprehensive education for dentists and doctors. Training programmes should emphasise that young people can and do get tongue cancer, even with the absence of traditional risk factors. Investment in research is also crucial. Innovations in diagnostic technology could streamline the process, making it more efficient and accessible. Fast and accurate diagnostic tools would reduce the reliance on resource-heavy and painful biopsies, allowing for more accurate diagnosis and earlier intervention.
Written consent was obtained from all patients named in this article. Thank you to those patients for their involvement.